2025 AGENDA
8:00 a.m. to 8:45 a.m.
8:45 a.m. to 8:55 a.m.
8:55 a.m. to 9:05 a.m.
9:05 a.m. to 9:15 a.m.
9:15 a.m. to 9:50 a.m.
9:50 a.m. to 10:25 a.m.
10:25 a.m. to 10:40 a.m.
10:40 a.m. to 11:15 a.m.
11:15 a.m. to 11:50 a.m.
11:50 a.m. to 1:15 p.m.
1:15 p.m. to 1:30 p.m.
1:30 p.m. to 1:55 p.m.
1:55 p.m. to 2:30 p.m.
2:30 p.m. to 2:55 p.m.
2:55 p.m. to 3:10 p.m.
3:10 p.m. to 3:35 p.m.
3:35 p.m. to 4:10 p.m.
4:10 p.m. to 4:25 p.m.
4:25 p.m. to 4:30 p.m.
4:30 p.m. to 4:35 p.m.
Registration and Breakfast
Opening Remarks – Kimberly Romo, Master of Ceremonies
Welcome – John Garcia, Arizona Biomedical Research Centre Program Director
Host Agency Address – Jennie Cunico, Arizona Department of Health Services Director
Roger Horton, PhD, Anthony Nolan Project UK
AABB Accreditation – What Does it Do? Christina Celluzzi, PhD, MS, CABP(H)
(Association for the Advancement of Blood & Biotherapies)
Break
Past-Present-Future of Cord Blood Collection & Research – Dr. Joanne Kurtzberg, MD, Duke University
Current Cord Blood Technology and Careers – Dr. Colleen Delaney, MD, MSc, Fred Hutch
Lunch
- Collector Breakout – Dr. Suzanne Pontow, MD, University of California – Davis, Erin Eaton,
MD Anderson Cord Blood Bank - Cord Blood in Classroom Breakout Charis Ober, Save the Cord Foundation; Melanie Hall, Save the Cord
Foundation; Kylee Cook, Arizona Public Cord Blood Program; Dr. Coleen Delaney, MD, MSc, Fred Hutch
Awards – John Garcia, MBA, Arizona Biomedical Research Centre Program Director and Victor Waddell, Arizona Biomedical Research Centre Executive Director
Cord Blood Banking in Canada – Dr. David Allan, MD, Univ. of Ottawa – Canadian Blood Services
Education Program Update – Melanie Hall, Save the Cord Foundation, and Charis Ober, Save the Cord Foundation
The Nurse’s Role in Cord Blood Collection – Joan Snelz, MSN-Ed, RNC-OB, BSN (NAU)
Break
Survivor Story – Eseosa Evbuomwan (Sickle Cell Survivor)
Cord Blood Transplantation: Addressing Allograft Access Disparities & Mitigating Relapse in High-Risk Disease – Dr. Warren Fingrut, MD, MD Anderson Cancer Center, Houston, TX
Call to Action – Dr. Colleen Delaney, MD, MSc, Fred Hutch
Closing Remarks – Victor Waddell, Ph.D., Arizona Biomedical Research Centre Executive Director
Last Word – Kimberly Romo – 2026 Save the Date Announcement
2025 SPEAKERS
Charis Ober
Charis Ober is the Founder and Executive Director of Save The Cord Foundation, a United States-based 501(c)(3) non-profit charity. She is a global advocate for umbilical cord blood education, awareness, research and legislation. Mrs. Ober is a graduate of the University of Arizona and has more than 25 years of experience in pharmaceutical and biotech sales, marketing and product development. Mrs. Ober lives in Tucson, Arizona with her family.

Suzanne Pontow, Ph.D.
Dr. Suzanne Pontow is the Co-Director of the Umbilical Cord Blood Collection Program at the University of California (UC) Davis Health System, where she is responsible for overseeing the collection and processing of umbilical cord blood samples. Dr. Pontow received her BS in General Sciences from University of Iowa in 1985, and her Ph.D. in Cell and Molecular Biology from Washington University School of Medicine in 1995. After 11 years studying how HIV infects cells, Dr. Pontow joined the laboratory of Jan Nolta, PhD, Director of the Institute for Regenerative Cures. The move to UC Davis allowed Dr. Pontow to pursue an interest in the remarkable stem cells that are routinely discarded with the placenta and umbilical cord following birth. In 2010, Dr. Pontow and Jon Walker, CLS were named Co-directors of the Umbilical Cord Blood Collection Program for the state of California, which is administered from the UC Davis Health System.
Dr. David Allan
Dr. David Allan is a Professor of Medicine at the University of Ottawa and a transplant hematologist at the Ottawa Hospital. In addition, he is a medical director for Stem Cells at Canadian Blood Services which runs an unrelated donor registry and public cord blood bank to support transplantation and cellular therapy. His research focuses on knowledge synthesis in regenerative medicine, to accelerate novel technologies in cell therapy and transplantation, and to improve access to optimal donors in hematopoietic cell transplantation.

Melanie Hall
Melanie Hall serves as Director of Education Outreach at Save the Cord Foundation, a 501(c)(3) non-profit charity. As content designer of a curriculum aimed at increasing awareness and interest in cord blood stem cells, Melanie brings a unique blend of analytical thinking and innovation to her work, consistently seeking creative solutions when promoting initiatives. With a dedicated focus on enhancing the human experience in healthcare, Melanie works at Mayo Clinic as a contributor on the patient experience team. Earning her B.S. in Healthcare Administration from Brigham Young University - Idaho, Melanie has over 12 years in non-profit leadership, marketing, program development and management, and promotion.
Dr. Warren Fingrut
Dr. Warren Fingrut is an Assistant Professor with the Department of Stem Cell Transplantation and Cellular Therapy at The University of Texas MD Anderson Cancer Center in Houston, Texas. His research focuses on characterizing and addressing disparities in access to transplantation. He previously completed BMT Fellowship at Memorial Sloan Kettering Cancer Center in New York, where he trained in Cord Blood Transplantation under the mentorship of Juliet Barker. He also received his Master of Public Health from the Harvard T.H. Chan School of Public Health.

Dr. Joanne Kurtzberg
Dr. Kurtzberg is an internationally renowned expert in pediatric hematology/oncology, pediatric blood and marrow transplantation, umbilical cord blood banking and transplantation, and novel applications of cord blood and birthing tissues in the emerging fields of cellular therapies and regenerative medicine. Dr. Kurtzberg serves as the Director of the Marcus Center for Cellular Cures (MC3), Director of the Pediatric Transplant and Cellular Therapy Program, Director of the Carolinas Cord Blood Bank, and Co-Director of the Stem Cell Transplant Laboratory at Duke University. The Carolinas Cord Blood Bank is an FDA licensed public cord blood bank distributing unrelated cord blood units for donors for hematopoietic stem cell transplantation (HSCT) through the CW Bill Young Cell Transplantation Program. The Robertson GMP Cell Manufacturing Laboratory supports manufacturing of RETHYMIC (BLA, Enzyvant, 2021), allogeneic cord tissue derived and bone marrow derived mesenchymal stromal cells (MSCs), and DUOC, a microglial/macrophage cell derived from cord blood. Dr. Kurtzberg’s research in MC3 focuses on translational studies from bench to bedside, seeking to develop transformative clinical therapies using cells, tissues, molecules, genes, and biomaterials to treat diseases and injuries that currently lack effective treatments. Recent areas of investigation in MC3 include clinical trials investigating the safety and efficacy of autologous and allogeneic cord blood in children with neonatal brain injury – hypoxic ischemic encephalopathy (HIE), cerebral palsy (CP), and autism. Clinical trials testing allogeneic cord blood are also being conducted in adults with acute ischemic stroke. Clinical trials optimizing manufacturing and testing the safety and efficacy of cord tissue MSCs in children with autism, CP and HIE and adults with COVID-lung disease are underway. DUOC, given intrathecally, is under study in children with leukodystrophies and adults with primary progressive multiple sclerosis. In the past, Dr. Kurtzberg has developed novel chemotherapeutic drugs for acute leukemias, assays enumerating ALDH bright cells to predict cord blood unit potency, methods of cord blood expansion, potency assays for targeted cell and tissue based therapies. Dr. Kurtzberg currently holds several INDs for investigational clinical trials from the FDA. She has also trained numerous medical students, residents, clinical and post-doctoral fellows over the course of her career.

Christina Celluzzi Ph.D., MS, CABP(H)
Dr. Christina Celluzzi has a background in biomedical research which includes basic and applied research in cellular therapy (CT). She holds BS and MS degrees in Microbiology and earned her PhD in Medical Sciences at the University of Nijmegen in The Netherlands where she studied malarial immunity. Her entry into cellular therapies began with seminal research at the University of Pittsburgh investigating the role of dendritic cells (DC) in cytotoxic T-lymphocyte induction in melanoma. She continued in CT with the development of DC closed-culture systems and supporting assays for clinical application as research scientist and faculty member at the American Red Cross Holland Biomedical Laboratory and University of Maryland School of Medicine. She applies her more than 30 years of experience to her current position at AABB serving as a resource to its many CT professionals – helping to create and develop projects, including the Cellular Therapies Certificate Program, as well as other activities for the biotherapies professional.

Roger Horton, Ph.D.
Roger Horton is the FACT Director of the Anthony Nolan Cord Blood Bank and Cell and Head of Clinical Innovation and Partnerships at the Anthony Nolan Cell Therapy Centre in Nottingham, UK. He also acts as a person designate for the Human tissue Authority, which is the UK regulator. He has been a FACT Cord Blood Bank Inspector since 2016 and serves on a number of committees, including the FACT CB Standards Committee, Accreditation Committee and the CBA Education Committee as well as being part of the WMDA cord Blood working group. He has more than 17 years’ experience in the field of cord blood, stem cells, cellular therapy and leukaemia and, as part of the Cord Support Programme in the UK, is passionate in promoting best practice in the search, selection, manufacture and application of cord blood in both transplant and cellular therapy applications.

Erin Eaton
With over 25 years of experience in operations management, human resources, strategic planning and business development. Since 202, Erin has served as the Manager for Cord Blood Bank Operations at MD Anderson Cord Blood Bank in Houston, Texas. Ms Eaton has been a key force in expanding the Cord Blood Bank (CBB) at MD Anderson Cancer Center and has been instrumental in the success of strategic partnerships with groups such as the Arizona Public Cord Blood Program. Likewise, she holds a leading role in ensuring that the CBB operations are in accordance with the FDA, HRSA, NMDP, FACT, CAP and CLIA requirements, guidelines, and standards.

Joan Snelz, MSN-Ed, RNC-OB, BSN
Joan Snelz is currently serving as an Assistant Clinical Professor at Northern Arizona University. Previously Joan worked as a Registered Nurse for Banner Health and served in the roles of a nurse coordinator, and as a patient and family educator. Ms. Snelz was responsible for assessing and triaging OB/Gyn patients appropriately based on primary complaint. She provided education regarding labor signs/symptoms, common discomforts of pregnancy, postoperative restrictions or concerns, gynecologic concerns, medication safety, and normal postpartum course. Additionally, she Assessed patients based on standing orders and notify providers as appropriate for any questions or concerns. Joan received her Master of Science in Nursing, specializing in nursing education, from Grand Canyon University. She received a Bachelor of Science degree in Nursing from Indiana University in Indianapolis and a Bachelor of Science in Early Childhood Education and Teaching from Purdue University.

Dr. Colleen S. Delaney, MD, MSc
Colleen Delaney, MD, MSc, is an attending physician at Seattle Children's Hospital; director of the Cord Blood Transplant Program and associate professor in the Clinical Research Division at Fred Hutchinson Cancer Center; and associate professor at the University of Washington School of Medicine. Dr. Delaney's research interests include hematopoietic stem cell regulation and the development of novel and clinically feasible ex vivo expansion systems for hematopoietic progenitor cells using the Notch ligand, Delta1, which is a known regulator of cell fate determination. Her goal is to improve the outcome of patients in need of a cord blood transplant. Delaney's research on the role of Notch signaling in hematopoietic stem cell regulation has resulted in the development of a pilot study investigating the use of ex vivo expanded cord blood progenitors to augment conventional cord blood transplantation. She is lead investigator in this trial, which began accrual in summer 2006. Delaney is principal investigator on four additional Fred Hutchinson clinical trials investigating the use of single or double unrelated donor umbilical cord blood grafts as an alternative source of stem cells for hematopoietic cell transplant, including a multicenter protocol investigating the use of single versus double unrelated donor umbilical cord blood grafts as the source of stem cells for hematopoietic cell transplantation. Dr. Delaney is Board Certified in pediatric hematology-oncology. She received her medical degree from Harvard Medical School, Boston, MA. Her research focus area is stem cell transplantation, and translational research.
CORD BLOOD TRANSPLANT SURVIVOR

Eseosa “Sosa” Evbuomwan
Eseosa “Sosa” Evbuomwan is a 2021 graduate of the University of North Carolina at Chapel Hill, currently working in healthcare while completing the necessary coursework to apply to medical school. With a deep passion for medicine, Sosa’s journey in healthcare is deeply personal—she was born with sickle cell anemia, a condition that once defined her world. In 2012, she made history as the first pediatric patient in the world to be cured of sickle cell disease through a double ni-cord cord blood transplant. Since then, she has been determined to embrace every opportunity life has to offer. She shares her story about her cord blood transplant frequently and has worked alongside multiple organizations including Duke Hospital, Be The Match, and the AZ Public Cord Blood Program! Beyond her medical aspirations, Sosa is an adventurer at heart. She loves reading, traveling, public speaking, staying active, and—more recently—content creation. Never one to shy away from a challenge, she even stepped onto the pageant stage as a competitor in Miss NC USA 2023! Her personal story fuels her advocacy for cord blood and stem cell research, and she remains committed to uplifting minority communities through her work. In everything she does, Sosa strives to make her 12-year-old self-proud—turning her resilience into a force for change and inspiration.

CONFERENCE HOST SPEAKERS

Jennifer Cunico, MC
Jennifer (Jennie) Cunico is the Director of the Arizona Department of Health Services (ADHS). Jennie has been with the agency since 2014. During this time, she has served in multiple leadership roles, including Deputy Director for Public Health Planning and Operations, where she oversaw policy development, hiring professional and support staff, information technology, business intelligence, data management, workforce and professional development, community engagement and the department’s budget. Prior to joining ADHS in 2014, Jennie worked in the private sector overseeing office operations for a successful small business for 15 years. In addition, Jennie worked in Arizona’s behavioral health system at a local non-profit for 10 years. She holds a Bachelor of Science in Psychology from Arizona State University and a Master of Counseling with an emphasis in Marriage and Family Therapy from the University of Phoenix.

Dr. Victor Waddell
Victor Waddell, Ph.D., is the Director of the Arizona State Public Health Laboratory and Executive Director for the Arizona Biomedical Research Center which includes the Arizona Public Cord Blood Program. Dr. Waddell earned his doctorate in Molecular Biology and Genetics at Queen’s University Belfast, N. Ireland. His other degrees include a Master of Science in Environmental Sciences and a Bachelor of Science in Biological Sciences also from Queen’s University Belfast. He has published many articles relating to both Public Health and Molecular Biology. Dr. Waddell has worked for the Arizona State Public Health Laboratory since 2001, and is responsible for overseeing the entire laboratory including the Chemistry, Microbiology, Newborn Screening, BioEmergency Response, and Chemical Emergency Response Sections at the State Laboratory. Dr. Waddell served as President of the Association of Public Health Laboratories from 2011- 2012 and is currently President of the Clinical Laboratory Standards Institute.

Mr. John Garcia, MBA, CPM
Since 2020, John Garcia has served as the Program Director of the Arizona Biomedical Research Centre (ABRC). Mr. Garcia oversees the distribution of grant funds to biomedical researchers and to Arizona universities to educate their faculty, staff, students, and the public. He also manages the Arizona Public Cord Blood Program. He earned a Master of Business Administration with an emphasis in Information Technology Administration from University of Arizona Global Campus (formerly Ashford University). Mr. Garcia also completed a Bachelor of Arts degree in Management with the University of Phoenix. Additionally, he also received certification as a Public Manager through Arizona State University. His career in public service spans 40 years. John's work includes information technology, grant administration, public policy, budget, finance, and criminal justice administration.

Kimberly Romo, Master of Ceremonies
Kimberly Romo is currently the Director of Business Operations for Marana Health Center Healthcare, also known as MHC Healthcare, where she oversees 17 community health clinics. She is proud to have served on the Save the Cord Foundation board for more than a decade. A native of Tucson, Kimberly spent the first 11 years of her career as a broadcast journalist before transitioning to healthcare in 2012. Since then, she has spent time in the acute, post-acute and behavioral health space where she leveraged her vast experience in communications, media relations, business development and revenue operations to drive companies forward. Helping establish Arizona's first public cord blood donation program at Tucson Medical Center remains one of her proudest professional accomplishments.
Get our official event app,
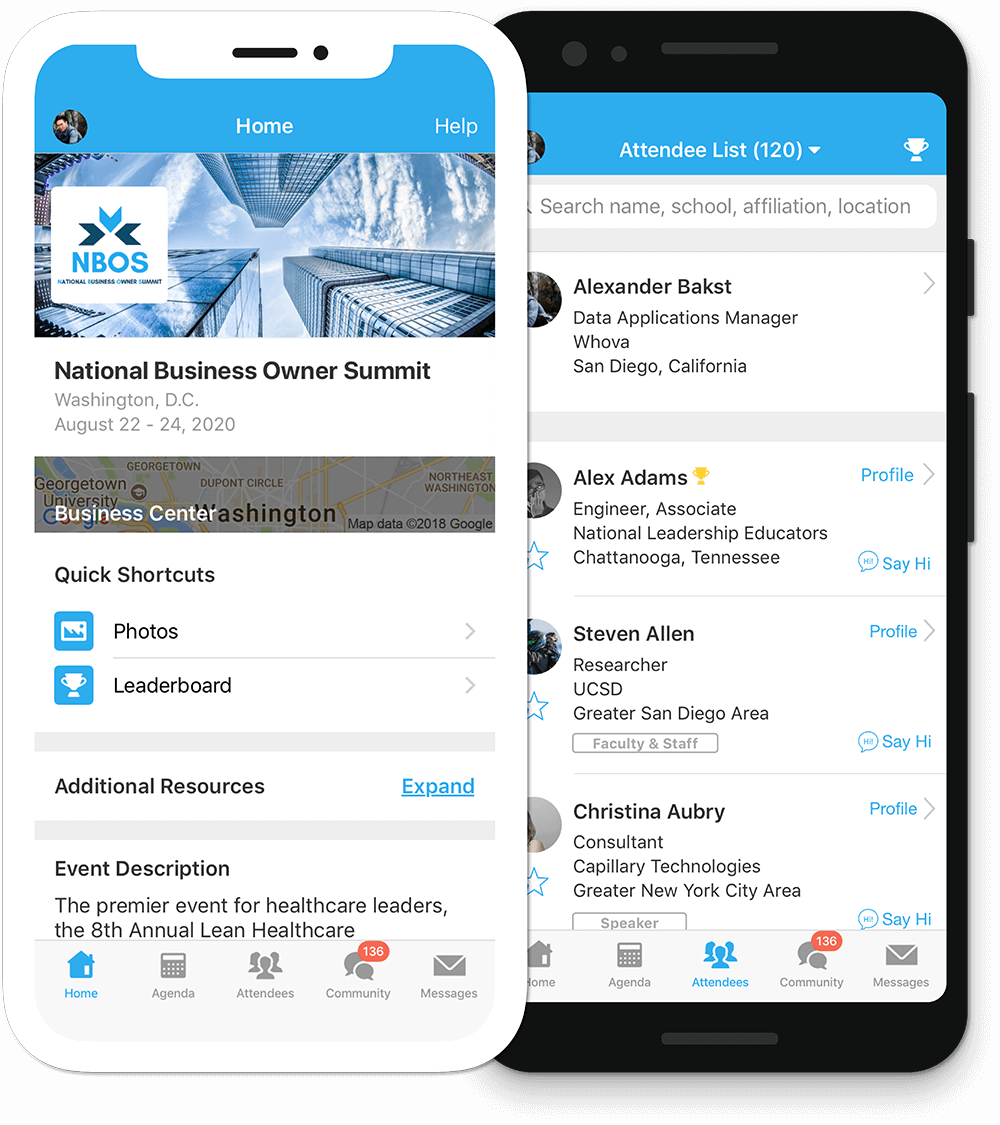
Get the most out of the app and have a more productive experience!
1
NAVIGATE the event agenda and logistics, even without Wi-Fi or data. Access useful information like ridesharing and local attractions through the Community Board
2
NETWORK effectively. Plan whom to meet by exploring attendee profiles and sending out messages
3
PARTICIPATE in event activities through session likes, comments, ratings, live polling, tweeting, and more
For Blackberry or Windows Phone, Click here
For feature details, visit Whova
ABOUT US
Umbilical cord blood is blood that remains in the blood vessels of the placenta and the umbilical cord, and is collected after the baby is born and the cord has been clamped and cut. Cord blood can be used much the same way that bone marrow stem cells are used for a life-saving transplant. For many patients in need, a cord blood transplant is the best or only hope for a cure. Donating umbilical cord blood is free, painless and neither mother nor child is harmed in the collection. The Arizona Biomedical Research Centre currently funds four collection hospitals, Save the Cord Foundation, and the cord blood bank with lottery revenue to make the program possible.
Today, cord blood can be publically collected, stored, and made available for transplant to children and adults for the treatment of more than 80 life threatening diseases such as certain genetic and metabolic diseases, blood cancers such as leukemia and lymphoma, and sickle cell anemia.
38% of African Americans,
31% of Native Americans,
27% of Hispanics,
12% of Caucasians and
51% of Native Hawaiian or other Pacific Islanders rely on cord blood transplants.
Many people are still unable to find a match.
Adding diverse units of umbilical cord blood to the registry increases the likelihood that all patients will find a match.
have been used in transplants to treat or cure life-threatening diseases and hundreds of cord blood units have been banked and listed on the registry for potential transplantation.
The MD Anderson Cord Blood Bank is licensed by the FDA and accredited by FACT as a public cord blood bank. The bank is managed by immunogeneticists and stem cell transplant physicians who have decades of experience in the field.
Save the Cord Foundation is a 501c3 non profit, which was established to promote awareness of the life-saving benefits of cord blood based on unbiased, factual information. The foundation educates parents, health professionals, students and the general public about the need to preserve this valuable medical resource. The foundation provides information on cord blood research, and both public cord blood donation programs and private family cord blood banks worldwide.
CONTACT US
Feel free to get in touch with us by sending us an e-mail at:
cordbloodInfo@azdhs.gov
PARTNERS